Electronic Health Records (EHRs) have had their fair share of criticism. Many primary care physicians (PCPs) felt they were more of a hurdle than a help, disrupting workflows and exacerbating administrative burdens.
Today, the outlook has shifted. As of 2021, nearly 9 in 10 (88%) U.S. office-based physicians have adopted EHR systems. Valued at $11.38 billion in 2023, the U.S. EHR market is projected to grow at a 2.24% CAGR through 2030. This transition reflects a growing understanding of EHR's true potential.
EHRs can empower or overwhelm; it’s all about your approach. Successful implementation makes all the difference. Let’s explore how optimized, EHR-driven strategies can become the ultimate catalyst for boosting patient engagement.
EHR systems were built to streamline clinical data management, but have transformed into a central digital healthcare tool that enhances patient engagement. Far from being just a clinical data storehouse, it now connects providers with their patients, offering insights into clinical indicators, risks, and opportunities to personalize care.
Personalized care is the future of medicine. Tailored treatments, communications, and care plans create a unique and meaningful experience that makes patients feel seen, heard, and valued. It builds trust, encourages patients to take ownership of their health, and improves patient engagement. Here's how you can leverage EHR to develop a patient engagement strategy.
Many patients struggle to understand their health conditions. According to the Center for Health Care Strategies (CHCS), 9 in 10 adults in the United States struggle with health literacy. Another study by the American Academy of Physician Associates (AAPA) reveals that 40% of adults admit they sometimes hesitate to speak up during appointments, a challenge frequently encountered by individuals with limited literacy.
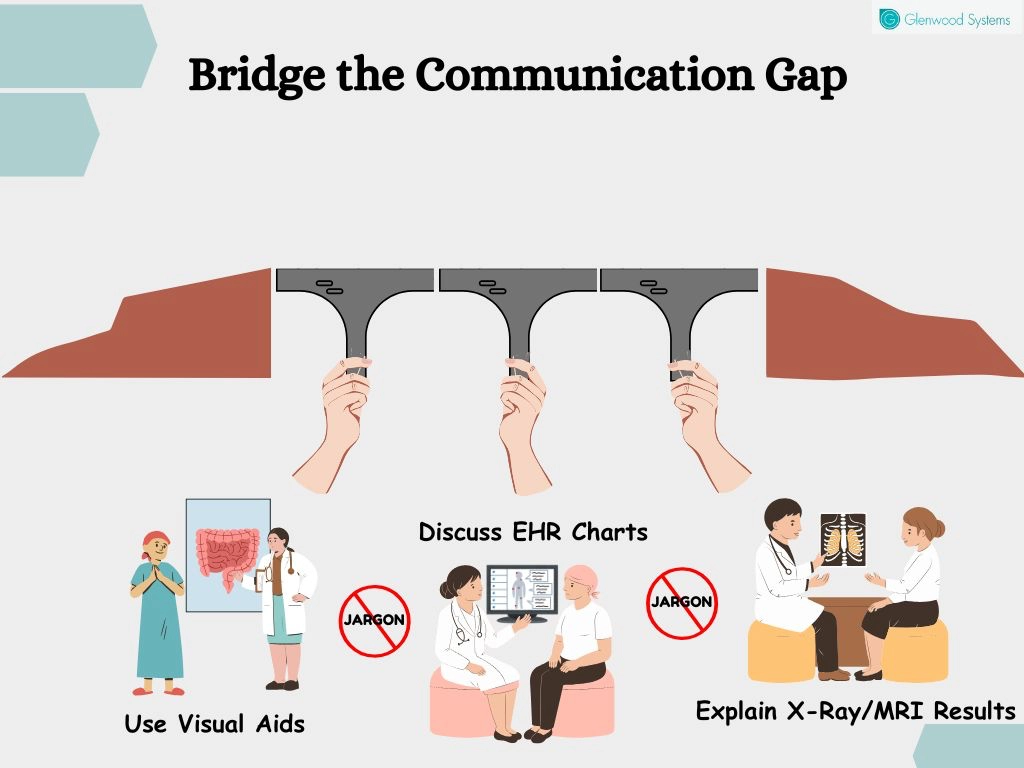
Health literacy is a critical issue that has a direct impact on health outcomes. Patients who lack a clear understanding of their condition or treatment are more likely to miss follow-ups, not adhere to medications, or struggle to manage chronic conditions. Making consultations visually interactive can effectively bridge this gap.
Visual aids, such as EHR charts, graphs, and images, can transform complex information into understandable insights. You can use these to discuss X-rays, MRIs, or other imaging results with patients and clarify findings. Use animations to demonstrate how medications or treatments work and, most importantly, pair visual tools with clear, jargon-free explanations.
For primary care physicians or family doctors with a long-standing relationship with their patients, personalizing care plans comes naturally — they’re familiar with medical histories, preferences, and previous treatments. However, creating a personalized care plan for a new patient is a different challenge. In such cases, having access to a comprehensive medical history is imperative. This is where interoperable EHRs prove invaluable.
EHR systems consolidate patient health information (PHI) from various providers, offering a holistic view of the patient’s medical journey. This integration gives providers insights into existing health conditions, previous treatments, and outcomes. A comprehensive medical history allows them to identify what has worked, what hasn’t, and what may pose risks, such as known allergens or adverse drug reactions.
Interoperability breaks down silos in care. For instance:
Tailored plans address the patient’s unique needs, improve health outcomes, and elevate patient satisfaction.
Timely access to care is critical, as delays or gaps can worsen a patient’s health condition, sometimes with fatal consequences. However, even more concerning is that more than 400,000 Americans lose their lives each year due to preventable medical errors, including medication-related errors.
Often, patients struggle to recall key details about their medical history, such as past illnesses, medications, or allergies, which creates a dangerous gap. Physicians unaware of these critical factors may unintentionally prescribe medicines that conflict with existing treatments or trigger allergic reactions that can turn fatal.
EHRs become lifesavers, generating a comprehensive and up-to-date medical record that gives you a holistic view of a patient’s health history. EHR systems flag potential conflicts between new and existing medications, alert known allergies, and ensure that recommendations and prescriptions are accurate, safe, and aligned with the patient’s ongoing treatments. Physicians can use EHR insights to engage patients in managing their conditions, particularly in cases of comorbidities.
EHRs are a comprehensive repository of your patient’s health data, providing critical insights beyond treatment planning. They are invaluable for the early detection of health disorders and for fostering preventive care.
For example, EHRs allow you to track a patient’s blood pressure trends over time. If the data reveals a pattern of increasing readings, it could signal early-stage hypertension. With this insight, you can proactively intervene by recommending lifestyle changes, prescribing medication if needed, and scheduling regular follow-ups to monitor progress.
EHR insights enable you to educate and engage patients in preventive care programs and wellness plans. Moreover, healthcare teams can craft personalized strategies to address risks, promote healthy habits, and prevent the onset of chronic illnesses, improving patient experience and outcomes.
Providers often make treatment decisions without involving patients. While well-intentioned, this top-down approach can alienate patients, especially in communities with varying lifestyles and customs. Treatment plans that fail to align with a patient’s daily life often lead to frustration and non-compliance.
For example, a non-native diabetic patient may struggle with a diet plan based on traditional Native American foods. A culturally relevant plan that incorporates familiar foods would be far more effective.
EHRs help bridge this gap, enabling clear communication about health conditions, treatment options, and care plans tailored to each patient’s lifestyle and values. Imagine a patient with hypertension following a diet high in salt. Instead of demanding they cut salt entirely, you can encourage them to swap high-sodium foods for healthier alternatives and suggest seasonings they enjoy.
Shared decision-making improves participation, makes treatment plans more practical, guarantees patient adherence, and strengthens the provider-patient relationship.
A study published in JAMA reports that providers spend around 36 minutes per visit on EHR documentation. That’s a significant chunk of time taken away from direct patient interaction. The more time spent on screens, the less face-to-face connection you have, which strains the patient-provider relationship.
Can you genuinely connect with someone who’s glued to a screen? No. Patients feel the same way.
When providers are busy documenting, patient engagement suffers, leaving many feeling unheard or rushed. Nearly half of patients report that their providers seem burned out, and two-thirds feel their appointments are rushed.
Advanced EHR systems with integrated AI technologies, such as voice recognition and virtual scribes (e.g., GlaceScribe), lighten the documentation load by recording patient-provider conversations and automatically generating SOAP notes. This automation allows you to focus on your patients without worrying about documentation. Moreover, these systems can also suggest ICD-10 diagnosis codes, recommend medications, and streamline workflows with custom shortcuts and templates.
The result? Faster documentation, less stress, more quality time with your patients, and improved patient engagement.
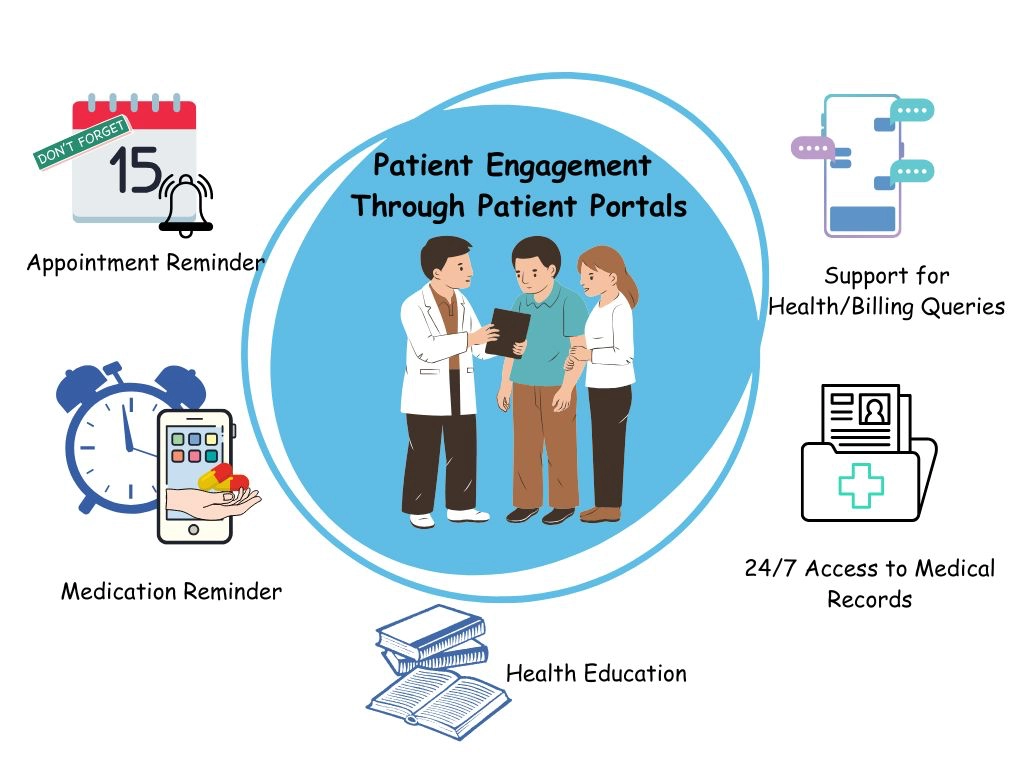
Patient portals are a valuable tool for engaging patients and encouraging active participation in their care. Statista reports that 96% of patients use their patient portals frequently or at least to some extent. Research also shows that patient engagement through portals increases medication adherence, improves health outcomes, and reduces emergency room visits.
Patient portals allow providers to send appointment reminders, medication alerts, and follow-up care instructions. Moreover, secure messaging facilitates timely responses to patient queries, improving satisfaction and trust. When critical information is easily accessible, it facilitates patient education and empowers them. Informed patients are more likely to follow treatment plans, attend scheduled visits, and feel connected to their care teams.
Teamwork in healthcare yields significant benefits, particularly for patients with chronic conditions or comorbidities who often consult multiple providers. An isolated approach fragments care, resulting in suboptimal health outcomes.
Collaboration instills a sense of family, where each team member works together to deliver comprehensive, coordinated, and efficient care. It's also critical during care transitions, such as hospital discharges or specialist referrals. EHRs centralize patient information, ensuring it's readily accessible when needed. Whether moving from hospital to home or from one specialist to another, EHRs ensure all care team members are on the same page with no gaps or redundancies in care.
Glenwood Systems offers innovative technological solutions — GlaceEMR, GlaceScribe, and GlacePhoneSmart — to streamline healthcare operations and reduce administrative burdens. Integrated with AI, our tools simplify documentation and enhance provider productivity, creating efficient workflows and seamless communication. We empower you to build stronger patient relationships, boost engagement, and ultimately improve health outcomes.
Schedule a Free Consultation!
