No-shows aren’t new; every healthcare provider has faced that frustrating gap in the schedule where a patient was supposed to be. More than an empty slot, it’s lost time, missed revenue, and a break in the continuity of care you work hard to provide.
In the U.S., the average patient no-show rate ranges from 6% to 23%. And with each missed visit costing around $200, no-shows drain nearly $150 billion from the healthcare system every year. That’s a massive dent in practice efficiency and revenue. Imagine what those dollars could mean if redirected toward improving access, technology, or patient experience.
Quick fixes and surface-level solutions may offer temporary relief but seldom deliver strong ROI. What your practice needs is a strategy that targets the root causes of no-shows. Join us as we explore 10 practical strategies that minimize no-shows and ensure your practice has a full schedule every day.
Waiting is rarely pleasant, and for patients who are already unwell, it can be frustrating and disheartening. Whether it’s the wait to schedule an appointment or the time spent in the waiting room, delays often lead patients to rethink (or skip) their visit.
According to the 2025 Survey of Physician Appointment Wait Times, scheduling an appointment slowed by 19% in 2024, with patients waiting an average of 31 days to see a physician across 15 major U.S. metro areas. That’s a whole month between a patient’s call and their consultation; enough time for symptoms to resolve, motivation to fade, or for them to find care elsewhere.
Reducing the gap between scheduling and the actual visit can make a measurable difference in lowering no-show rates. The sooner patients are seen, the less likely they are to drift away.
And it’s not just about booking delays, the in-office wait matters too. Research shows that patient satisfaction drops when actual wait times exceed expectations. Someone waiting an hour might not mind if they had expected a long delay, but another patient could feel frustrated if they had anticipated a quick visit and waited 30 minutes instead.
Setting clear expectations about wait times and creating virtual queues that allow digital check-ins can go a long way toward maintaining trust and reducing missed appointments. Additionally, having patients complete their digital forms ahead of time helps streamline the visit and gauge their likelihood of showing up.
When there’s too much time between scheduling and the actual visit, even the best-intentioned patients can miss their appointments. Research shows that 38% of patients who miss their appointments do so because they forgot. Fortunately, a friendly reminder is all it takes to turn that missed slot into a confirmed visit.
Sending reminders 24–48 hours before the appointment can significantly reduce no-shows. The key is to reach patients through their preferred communication channel, whether that’s text, email, or phone.
But here’s where many practices stumble: one-way reminders or portals that are hard to access only add digital friction. In a recent MGMA poll, 73% of medical practices that have successfully reduced or stabilized their no-show rates attribute it to offering easy cancellation and rescheduling options.
Patients want convenience, not hurdles. Use a two-way texting that lets them confirm, ask a quick question, or even “tap to reschedule.” For high-risk appointments, including new patients, procedures, or imaging that requires prep, follow up with a live call if there’s no response.
The traditional “call-the-front-desk” approach to scheduling might have worked years ago, but today patients expect more flexibility. Waiting on hold or playing phone tag to book an appointment is frustrating.
Self-scheduling gives patients autonomy and reduces scheduling friction. It empowers them to book appointments anytime (even outside office hours) and pick a slot that actually fits their day. Beyond convenience, self-scheduling tools lighten administrative load on front-end staff and reduce scheduling errors. When patients feel in control, they’re more likely to show up.
Additionally, a highly effective strategy is to ask patients at the time of scheduling whether they’d like to be notified if an earlier appointment becomes available. Maintaining a waitlist of flexible patients enables your practice to fill in cancelled slots, keep the schedule full, and offer patients the opportunity for an earlier consultation.
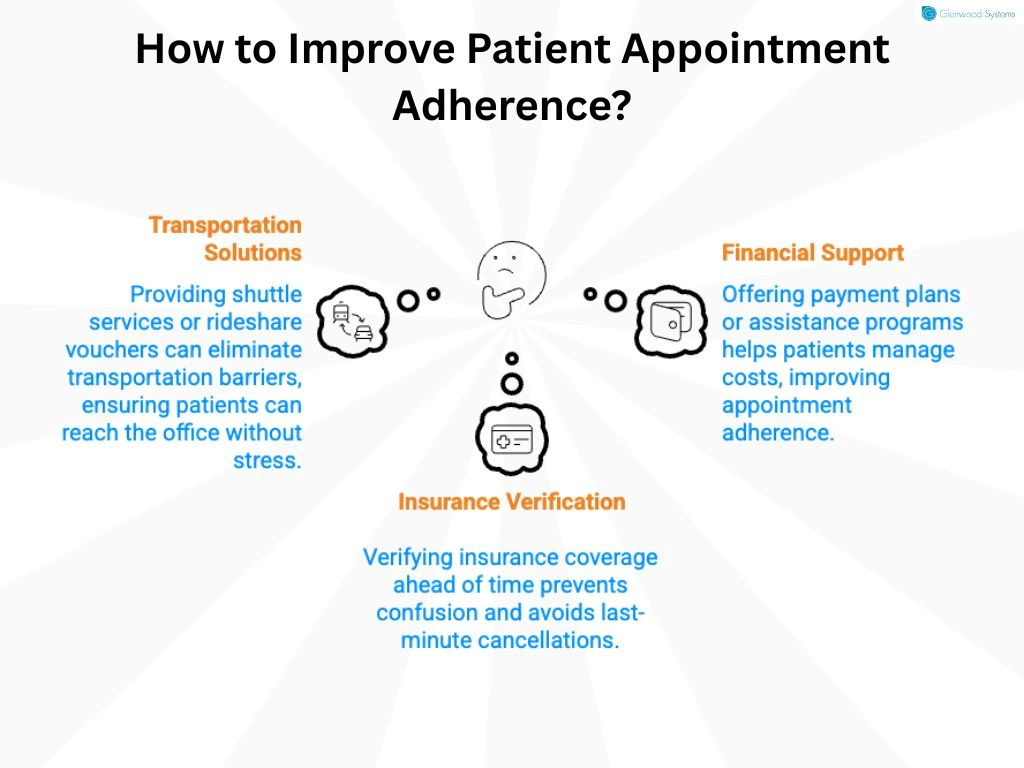
Most patients don’t intentionally miss appointments. Often, practical barriers stand in the way of the care they urgently need. Transportation challenges, medical debt, copay costs, and insurance limitations are common reasons for no-shows.
Research by the Robert Wood Johnson Foundation reports that 21% of adults who don’t have access to a vehicle or public transportation forgo needed care. In these situations, simply rescheduling an appointment or shortening wait times isn’t enough; you need to address the root cause.
Here are a few practical ways to help remove barriers and make it easier for patients to keep their appointments:
Patients want to feel cared for and valued. When they know you’re genuinely listening and paying attention to their needs, they’re less likely to miss the appointment and adhere to their treatment plans.
Simple gestures, such as remembering a patient’s preferences, checking in after a procedure, or answering questions with patience, can make a huge difference.
Communication is the foundation of a strong provider-patient relationship. It’s not about giving instructions; it’s about listening, showing empathy, and sending reminders that feel personal, not robotic. When patients feel supported, they’re more engaged, loyal, and are less likely to miss an appointment.
Telehealth removes many of the barriers that lead to patient no-shows. For those who struggle with transportation or mobility challenges, or who have busy schedules, a virtual visit makes it easy to stay on track with their care.
However, telehealth delivers the best results when used strategically. It’s ideal for behavioral health visits, medication refills, chronic care management, and quick follow-ups that don't require an in-person exam. Thoughtfully leveraging telehealth reduces no-shows and frees up in-office slots for patients who need them.
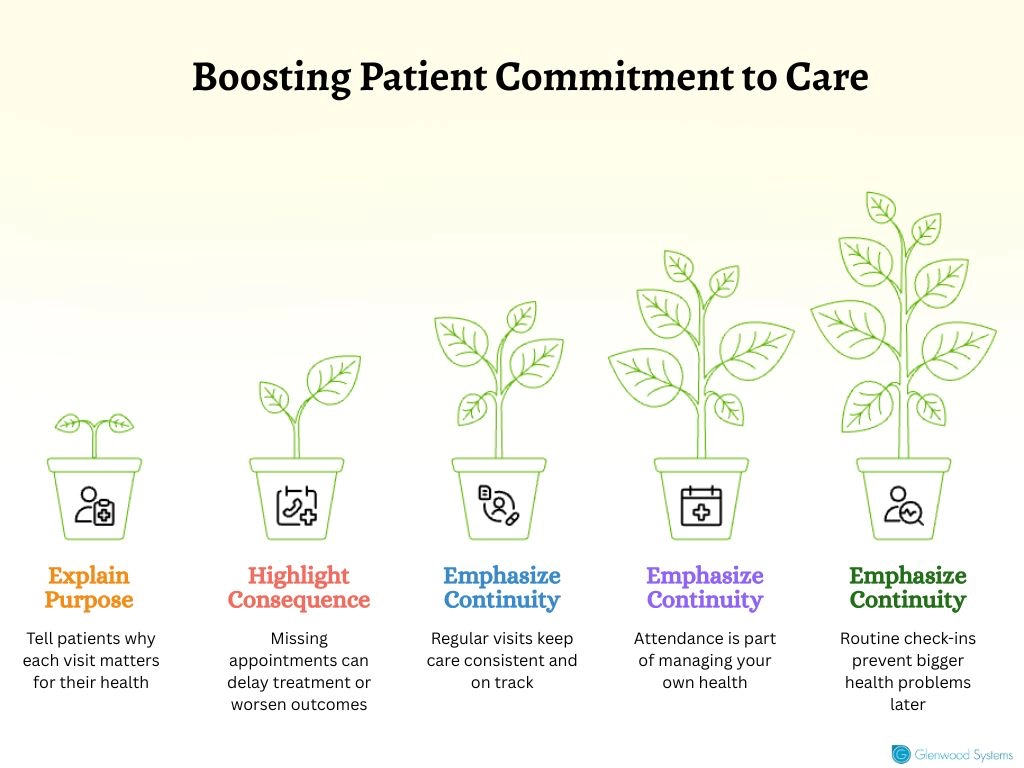
Many patients skip follow-ups or routine check-ups simply because they feel fine. If the symptoms have eased, they assume there’s no need to return, or they avoid appointments out of fear that “something bad” might show up. But missed visits often mean missed opportunities to catch issues early or track how well a treatment is working.
When patients know the purpose behind their visits, they feel more informed and less anxious about their consultation. Use plain language to explain how regular check-ins keep their treatment on track, ensure progress, and prevent health issues from escalating. You can also reinforce this through after-visit summaries or friendly reminders that connect the dots (“Your next visit will help us see how your new medication is working”).
No-shows don’t usually happen because patients don’t care; life sometimes gets in the way. For many working individuals, finding time during standard office hours is a challenge. Meetings run late, school pickups come up, or personal errands take priority.
Offering extended hours, like early mornings, late evenings, or weekends, gives patients the flexibility to fit healthcare into their busy lives. It also shows that your practice values their time.
Even small changes, such as keeping a few flex slots for same-day appointments, send a simple but powerful message: we care about making healthcare convenient for you. When patients have options that actually work for them, adherence improves, and loyalty follows.
Every corner of healthcare is feeling the impact of AI (Artificial Intelligence), including its power to predict no-shows. AI-driven models analyze patient data, appointment history, demographics, no-show behavior, and other factors to identify patients most likely to miss their appointment.
Several studies have demonstrated the effectiveness of AI-driven appointment systems. One model, for example, achieved 91% accuracy in predicting patient no-shows. In another study, healthcare organizations that adopted AI-based scheduling tools reported a 10% increase in monthly patient attendance, resulting in fuller schedules, reduced revenue loss, and improved continuity of care.
With AI's predictive power, you can proactively intervene, send targeted reminders, offer rescheduling options, or even flag high-risk appointments for additional follow-up. Don’t wait for patients to miss visits; take action to prevent no-shows.
Implementing a no-show fee is another strategy to minimize missed appointments. Practices that charge a no-show fee have seen measurable results, with a 25% improvement in attendance in 2024 compared to 16% in practices without a fee.
However, a poorly communicated no-show policy can confuse and negatively impact patient satisfaction. Ensure the policy is explained at the time of scheduling, included in appointment reminders, and visible on your website or patient portal. Clearly outline what counts as a missed appointment, the required notice for cancellations, and any associated fees.
Efficiency drives every successful practice, but no-shows hit the brakes hard. They disrupt schedules, drain resources, and jeopardize patient health outcomes. Understanding the root causes and proactively addressing them ensures your patients receive the care they need and that your schedule stays full.
Glenwood Systems’ practice management tools make this effortless. Our tools streamline scheduling, send automated reminders, and optimize every appointment, so you work at maximum efficiency. From reducing missed visits to enhancing patient communication, these solutions help your practice run smoothly, improve engagement, and keep patient care on track.
Schedule a Free Consultation!
