Ever had that sinking feeling when you log in to your billing portal and see the word 'denied' flashing back at you? Not again… – sound familiar?
Denials show up like uninvited guests, draining time, money, and morale. It doesn’t matter how many patients you’ve seen that week or how hard your staff worked to get claims out the door; even a single denial can set off a domino effect of phone calls, resubmissions, and frustrated sighs across the office.
These days, navigating the healthcare terrain is like playing a game where the rules keep changing mid-match. Denial rates are climbing, prior authorizations continue to stall care, and the surge in high-deductible plans is straining both providers and patients.
The impact is agonizing: cash flow gets squeezed while you pour hours into chasing payments that should already be in your pocket. But does that mean denials should be met with silence? Absolutely not! They’re not full stops; they’re opportunities to recover revenue.
With the right strategy, those “lost dollars” can be turned into steady, predictable revenue. That’s exactly what this 2026 playbook is about: tackling denials head-on, streamlining your revenue cycle, and showing you how to transform “Not again…” into “Paid in full."
Denials remain a persistent and growing challenge for providers. Nearly one in five in-network claims (19%) were denied under ACA Marketplace plans in 2023, with some insurers denying at even higher rates (54%). And that trend hasn’t slowed. The 2025 State of Claims report by Experian highlights that 41% of providers deal with denial rates of at least 1 in 10 claims.
Recent revenue cycle data from Kodiak Solutions paints an even clearer picture. Compared to 2023, providers in 2024 experienced slower payment processing from insurers, stretching already thin cash flow. At the same time, the initial denials rose by 2.4% to 11.81%, while the final denial rate remained relatively constant, increasing by 0.4%.
Adding to the burden, a recent HFMA survey revealed that half of healthcare leaders saw an increase in payer requests for information in 2024 compared to the prior year. Even more troubling, 47% reported that payer appeals now take nearly twice as long as they did just three years ago, delaying revenue recovery and compounding provider frustration.
There is, however, one sliver of relief: prior authorization burdens eased slightly, with authorization-related denials dropping by 7.7%. Still, that small win is quickly overshadowed by the bigger picture. In 2023, the average cost to fight a single denial was $57.23. At 100 denials a month, that’s more than $5,700 drained in lost time and resources. Denials may have changed shape, but they haven’t slowed down, leaving practices chasing dollars that should never have slipped through the cracks.
The 80/20 rule, also known as the Pareto Principle, is the idea that 80% of outcomes come from just 20% of causes. When it comes to denials, the math is no different. Roughly 80% of denials can be traced back to just 20% of recurring issues. Master those critical 20%, and you can prevent denials before they ever hit your portal, saving your practice hours of rework and thousands in lost revenue.
Here’s what makes up that 20%:
Many claim denials can be traced back to something deceptively simple: errors in eligibility and benefits verification. It’s a low-hanging fruit you can’t afford to miss. Too often, eligibility is checked only at the first visit, but that’s a risky approach. Nearly 3 in 10 consumers change their health plans each year, which means yesterday’s coverage may be invalid today.
Verifying eligibility at every single visit helps you catch coverage lapses and plan changes before a claim ever goes out the door.
Here’s how to get it right:
A few extra minutes of work early on can save hours of rework and resubmissions later. Plus, it strengthens patient trust and ensures they’re better prepared for the care ahead.
Prior authorization is one of the most common denial drivers, with 32.4% of healthcare leaders calling it the most challenging hurdle in revenue management. Most stem from one of two issues: either the prior authorization was never obtained, or the payer decided the service was “not medically necessary.” In both cases, the outcome is the same: lost revenue, wasted staff time, and frustrated patients.
An effective strategy is to build a bulletproof prior authorization process that removes assumptions and automates the otherwise tedious process:
Blending human vigilance with automation and AI-powered intelligence streamlines prior authorization, slashes denials, safeguards revenue, and ensures consistent cash flow.
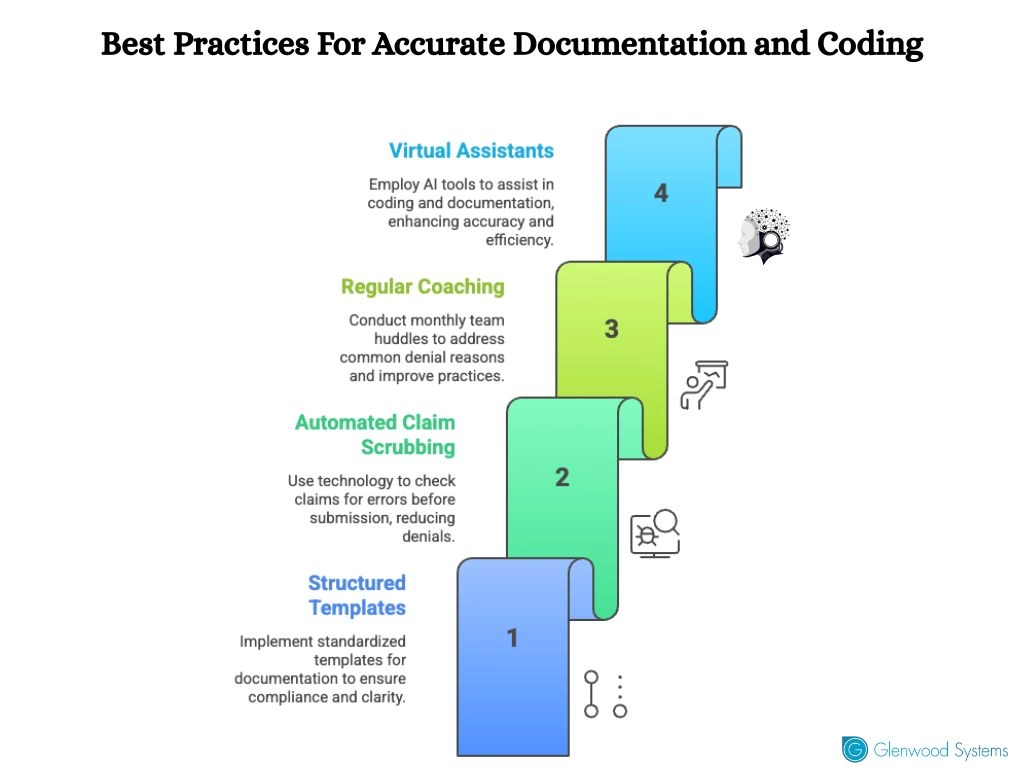
Documentation errors and coding slip-ups are denial magnets. A missing modifier, vague clinical notes, or inconsistent coding practices can derail an otherwise legitimate claim. The smallest oversight can mean the difference between fast payment and a lengthy appeal process.
Incorporate these best practices to tighten documentation and coding:
In claims submission, time is momentum. The faster you file a clean claim, the better your chances of first-pass acceptance and fewer draining follow-ups. Yet, delayed submissions remain one of the leading causes of preventable denials. Most payers enforce strict, timely filing limits, and once that window closes, reimbursement is almost impossible to recover.
Delays compound quickly: one late batch today becomes a week of unpaid claims tomorrow. It's time to approach claim submission like a daily discipline, not a weekly task. Submitting claims within 24–48 hours of service shortens A/R days, accelerates cash flow, and prevents backlogs that overwhelm your billing team.
Build operational rigor by designing workflows that prioritize same-day or next-day submissions, leveraging automation for claim batching, and deploying dashboards that flag aging claims before they near deadlines. Pair this with payer-specific alerts for timely filing limits, and you transform claims submission from a reactive process into a proactive revenue safeguard.
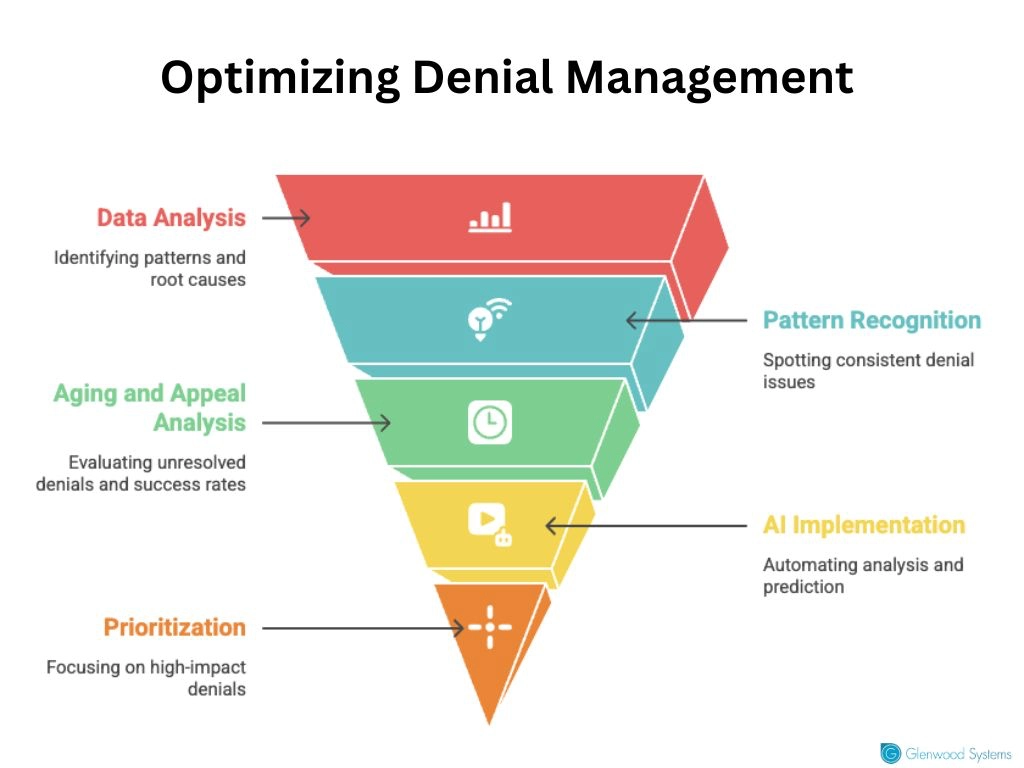
Every denial tells a different story. Some are tied to eligibility, others to coding errors, and still others to payer-specific quirks. If you’re not breaking down denials by payer, CPT/ICD code, provider, and location, you’re essentially flying blind.
Denial analytics uncover patterns that lead straight to the root cause. One payer may consistently reject a high-cost imaging code, or one provider may generate more request-for-information errors than the rest. Spotting patterns is vital to denial management.
Nevertheless, it's equally pivotal to dig into denial aging (how long denials remain unresolved) and appeal success rates to identify where your team is leaving money on the table.
Sifting through denial trends manually is error-prone and onerous. AI eliminates the manual grind and shifts the work from tedious number-crunching to proactive strategy building, so teams can focus on fixing issues rather than finding them. AI-powered analytics go beyond simple reporting; they can predict high-risk claims before submission, benchmark your denial rates against industry peers, and even suggest corrective coding or documentation in real-time.
Equally important, advanced analytics help you prioritize which denials to work on first. Not every denial carries the same financial impact, and 38% of healthcare leaders struggle to identify which ones matter most for revenue recovery and when to address them. Build dashboards that rank your top 10 denial reasons by both volume and dollar impact, so fixes are applied where they’ll drive the greatest financial return. Tackling this challenge ensures your team spends its time where it truly moves the bottom line.
Denials aren’t roadblocks; they’re data points. When tackled with the right strategy, they unlock faster cash flow and stronger financial performance. The future belongs to practices that don’t just manage denials but master them.
Glenwood Systems has long led the way in helping practices flip the script on denials by aiming for 99%+ collections and building denial resolution processes that are both fast and precise. Our partners across multiple specialties have seen an average revenue growth of 20%, proving that with the right systems in place, denial management becomes less about chasing dollars and more about capturing every dollar you’ve earned.
Turn denial challenges into cash flow wins and stay ahead of the curve. Let's partner to capture every dollar you’ve earned.
Schedule a Free Consultation!
