Clinical care may be the heart of healthcare, but it relies heavily on a parallel engine: administrative operations. Supporting every patient encounter is a network of essential tasks, including insurance verification, prior authorizations, claims processing, and payment reconciliation, all working quietly to ensure care is delivered and reimbursed on time.
These behind-the-scenes processes may be oblivious to patients, but they place a significant operational and financial strain on healthcare practices. And the numbers speak for themselves. According to the 2024 CAQH Index report, administrative activities in the U.S. healthcare system cost nearly $90 billion annually. A substantial share of this burden can be traced back to inefficient, manual, and disjointed processes that slow down operations and drain resources.
Fortunately, there’s a massive opportunity for improvement. Healthcare organizations can save nearly $20 billion annually by optimizing workflows and adopting automated, electronic solutions.
Is your RCM system broken? It's time to investigate what’s dragging it down and how you can get it back on track.
Revenue Cycle Management is the circulatory system of a healthcare organization; every function, from patient intake to final payment, is vital to maintaining optimum financial performance. When each step operates efficiently, revenue moves seamlessly. Contrarily, revenue cycle bottlenecks slow the system, leading to delays, lost income, and mounting strain.
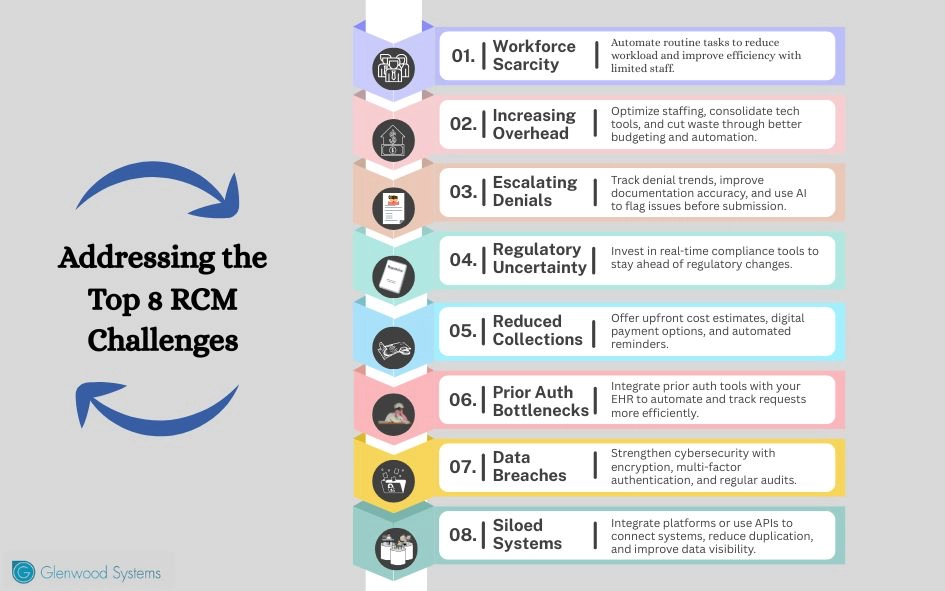
Running a healthcare business is challenging, even more so when your revenue cycle doesn’t run as smoothly as it should. Here’s a look at the top challenges that might be holding your revenue cycle back, and how to address them.
The Challenge:
Staffing shortage is a critical issue in healthcare, especially in private practices that lack the resources to absorb the impact. According to the Health Resources and Services Administration (HRSA), the U.S. is projected to experience a shortfall of over 187,000 full-time equivalent (FTE) physicians by 2037.
The strain also extends to administrative functions. The American Medical Association (AMA) reports a 30% shortage of medical coders, a gap that’s contributing to delays in claims, billing errors, and growing denial backlogs.
The Fix:
Traditional revenue cycle management is primarily manual and is unsustainable amid the ongoing workforce shortage crisis. The path to revenue optimization lies in automation. Many administrative tasks are repetitive, time-consuming, and prone to error. Automation handles routine processes, alleviates the burden, and enables staff to focus on high-value, complex work that demands human expertise.
Here are a few automation tools that lighten the load and fill the staffing gaps:
At Glenwood Systems, we bring these tools together into a unified platform and help simplify workflows, reduce administrative burden, and enable your team to do more with less.
The Challenge:
The upward trend in operating costs is forcing healthcare providers to reevaluate resource management and find more sustainable ways to operate. Labor alone accounts for 25%–30% of a healthcare organization’s revenue, while 30%–40% goes toward provider compensation.
In 2025, nearly 9 out of 10 practices reported an 11.1% increase in operating expenses compared to the previous year. Likewise, in a recent MGMA Stat poll, 65% of medical groups cited rising labor costs as a major concern, driven by inflation, workforce shortages, and fierce competition for skilled professionals. Nursing wages, in particular, have risen, with patient care assistant pay increasing by 12%, while certified nursing assistant compensation has surged by 38.4% over the past five years.
And that’s just one side of the equation. As organizations respond to growing cybersecurity threats and adopt AI-driven tools, technology spending is also climbing, adding to overhead.
The Fix:
The MGMA Stat poll revealed that 11% of medical practices that successfully reduced or maintained steady operating costs did so through a combination of tailored, data-driven strategies. These include optimizing staffing, investing in technology upgrades, improving inventory management, tightening expense controls, implementing disciplined budgeting, and renegotiating vendor/payer contracts.
These organizations didn’t rely on drastic cuts; they focused on aligning spending with value. That starts with identifying where costs are creeping up without delivering meaningful returns.
Are you paying for tools your team barely uses? Is manual labor driving up costs?
Taking a close look at what’s draining your resources is the first step toward building a financially resilient operation.
The Challenge:
Claim denials remain one of the most persistent and costly obstacles in revenue cycle management. They slow down cash flow and disrupt the day-to-day rhythm of practice operations. In 2024, nearly 6 in 10 medical groups reported an increase in denials. The most common culprits? Insufficient documentation, eligibility errors, incorrect patient information, untimely filing, and modifier mistakes. Many also faced rejections for prior authorizations, despite having initial approvals.
Constant shifts in payer rules and regulatory requirements have turned clean claim generation into a moving target. Concurrently, clinical and billing teams are stretched thin, juggling increased workloads with limited resources. The result? Delayed reimbursements, more resubmissions, and lost revenue.
The Fix:
Preventing denials is far more cost-effective than fixing them. First, monitor your denial patterns closely; understand the common triggers. Accuracy is non-negotiable. Establish robust feedback loops to help your team learn from errors, adjust workflows, and continuously improve.
For the denials that still slip through, have a well-structured rework process to recover lost revenue. Relying on manual efforts overwhelms your team, drags down productivity, and delays collections. Shift the heavy weight to technology.
AI-powered tools, including machine learning and predictive analytics, can flag high-risk claims and inaccurate codes before they’re submitted, allowing your team to correct issues upfront. Automated claim scrubbers also learn from past denials and spot documentation gaps, helping ensure cleaner claims.
Furthermore, automation lightens staff workload by taking over repetitive yet critical tasks such as eligibility verification, prior authorization tracking, and claim status updates. The result is fewer errors, smoother workflows, and more time for teams to focus on higher-value tasks.
The Challenge:
Healthcare regulations are constantly evolving, whether it's shifting CMS guidelines, new payer-specific rules, HIPAA guidelines, or surprise updates buried in policy bulletins. Staying compliant is like running on a treadmill that keeps speeding up. Miss a step, and it triggers claim denials, payment delays, audits, or financial penalties.
The Fix:
Don’t wait for changes to catch you off guard; stay proactive and build compliance into your daily operations. Invest in tools that track real-time regulatory updates across CMS, commercial payers, and state programs, so your team isn’t scrambling to adapt. Modern RCM software can monitor policy updates and automatically flag non-compliant claims, suggest coding corrections, validate documentation, and ensure your submissions align with the latest billing guidelines.
The Challenge:
In 2023, 41.7% of individuals under age 65 were enrolled in a high-deductible health plan (HDHP), primarily due to lower premiums. While these plans are appealing, they shift a greater share of financial responsibility directly onto patients. Rising out-of-pocket costs are fueling medical debt and straining collections for many practices.
Kodiak Solutions reported a decline in provider collection rates, from 37.6% in 2023 to 34.4% in 2024, highlighting the deepening challenges in revenue cycle management.
The Fix:
There’s an urgent need to redefine the patient financial experience. As more patients shoulder higher out-of-pocket costs, practices must adopt a patient-centered approach to billing and collections. That starts with clear, upfront cost estimates and flexible, digital-first payment options.
Experian’s State of Patient Access report found that 81% of patients say accurate cost estimates help them prepare for care, while 80% of providers agree it improves point-of-service collections. Paired with automated reminders for upcoming or overdue payments, these tools significantly improve cash flow and enhance patient experience.
Use plain, easy-to-understand language in your billing communications; skip the codes, abbreviations, and jargon. Making the payment process simple, transparent, and convenient encourages patients to comply with their financial responsibilities.
The Challenge:
Prior authorizations continue to be a massive time sink, delaying care and contributing to clinician burnout. According to the 2024 AMA Physician Survey, 9 in 10 providers report that prior authorization requirements lead to care delays, and 8 in 10 say they've seen patients abandon treatment as a result.
Clinicians and staff are spending an average of 13 hours per week managing prior authorization requests, with 90% linking it to burnout. While initial denial rates tied to prior authorizations dropped by 7.7% in 2024, the approval process remains tedious, fragmented, and time-intensive.
The Fix:
It’s time to automate, integrate, and optimize. Implement AI solutions that streamline prior authorizations within your EHR, verify payer rules instantly, provide real-time status tracking, and eliminate manual follow-ups.
Automation won’t eliminate prior authorization requirements, but it reduces administrative friction, frees up staff time, and helps ensure patients receive the care they need without unnecessary delays.
The Challenge:
Healthcare’s IT landscape is evolving. While this digital growth brings promising advancements that streamline operations, it also introduces new layers of complexity. The expanding web of interconnected systems, devices, and applications is making it increasingly challenging for IT and security teams to manage risks.
Cybersecurity has become a critical concern for healthcare providers. In 2024, cyberattacks compromised over 276 million PHI records, averaging 758,288 records daily. The massive data breach at Change Healthcare affected 190 million people, revealing the alarming scope of risk across the industry.
With vast amounts of sensitive clinical and financial data flowing through RCM systems daily, healthcare organizations are prime targets for cyberattacks. A single breach can erode patient trust, trigger costly fines, and damage your organization’s reputation.
The Fix:
Practices are bolstering their defences against cyberattacks. In 2024, 72% of medical group practices increased their cybersecurity investments, signaling a growing awareness of digital threats. Additionally, 7 in 10 medical group leaders say they feel very or somewhat confident in their ability to respond when these threats turn into active cyberattacks.
Embed cybersecurity into your revenue strategy. Start by enforcing end-to-end encryption, implementing multi-factor authentication, and conducting regular security audits to stay ahead of threats. Moreover, thoroughly vet your RCM vendors to ensure they maintain strong data protection protocols.
Finally, stay compliant with HIPAA regulations and updates; it’s a fundamental safeguard for your data, revenue, and reputation.
The Challenge:
Often, practice management systems operate in silos. The EHR may not communicate with the billing platform, clearinghouses function independently, and reporting tools pull data from multiple unconnected sources. This lack of system interoperability slows down operations, increases administrative burden, and creates data blind spots across the revenue cycle. Fragmentation also raises the risk of errors, delays, and revenue leakage.
The Fix:
It’s time to shift from silos to integrated systems. Invest in interoperable platforms or APIs to streamline workflows, reduce errors, and improve visibility. Integrated systems enhance data accuracy, accelerate claim processing, and optimize financial performance.
Revenue cycle challenges aren’t going away, but neither is the opportunity to fix what’s broken. The key lies in transforming healthcare RCM from a cost center into a powerful engine of growth.
GlaceRCM, Glenwood’s all-in-one revenue cycle solution, is designed with intelligent automation, real-time analytics, seamless EHR integration, and expert denial management to keep your operations running smoothly.
We’ll handle the admin burden. You can focus on care. Let’s talk.
Schedule a Free Consultation!
